| Aspect | Tubular Reabsorption | Tubular Secretion |
|---|---|---|
| Definition | Process of reclaiming essential substances from the ultrafiltrate back into the bloodstream. | Process of actively transporting certain substances from the bloodstream into the renal tubules. |
| Mechanisms | Passive diffusion, active transport, facilitated diffusion. | Active transport, counter-transport (antiport), passive diffusion. |
| Selectivity | Highly selective, retains essential substances, prevents waste loss. | Selective, focuses on waste removal, pH regulation, and maintaining electrolyte balance. |
| Location | Proximal tubules, loop of Henle, distal tubules, collecting ducts. | Proximal tubules, distal tubules, collecting ducts. |
| Regulatory Factors | ADH, aldosterone, ANP, PTH regulate reabsorption. | RAAS, acid-base balance, diuretics affect secretion. |
| Substances Reabsorbed/Secreted | Reabsorbs water, glucose, amino acids, ions (e.g., sodium, potassium, calcium, chloride), various solutes. | Secretes hydrogen ions (H+), creatinine, drugs, metabolic waste products, potassium ions (K+). |
| Clinical Significance | Impacts conditions like diabetes, hypertension, and edema. | Used to assess kidney function, manage acid-base imbalances, and drug excretion. |
| Primary Goal | Retains valuable substances, maintains body’s homeostasis. | Eliminates waste, regulates pH, controls electrolyte balance. |
| Efficiency | Highly efficient, reclaims most valuable substances. | Efficient in eliminating waste products and regulating pH. |
| Role in Fluid Balance | Influences fluid reabsorption, conserves water when needed. | Helps regulate water and electrolyte balance. |
| Typical Outcome | Concentrates the urine by reabsorbing water, electrolytes, and nutrients. | Excretes waste products and maintains proper pH and electrolyte balance. |
| Example Processes | Reabsorption of glucose, sodium, and amino acids. | Secretion of hydrogen ions (H+), creatinine, and some drugs. |
| Impacts Drug Elimination | May affect drug reabsorption from the renal tubules. | Critical for excreting drugs and preventing drug accumulation. |
| Hormones Involved | ADH, aldosterone, ANP, PTH influence reabsorption. | RAAS system, acid-base balance hormones, diuretics influence secretion. |
| Maintenance of Blood Pressure | Influences blood pressure by regulating sodium reabsorption. | Impacts blood pressure through the regulation of blood volume. |
| Role in Acid-Base Balance | Minor role in maintaining blood pH. | Major role in regulating blood pH by secreting or reabsorbing hydrogen ions (H+). |
| Primary Waste Elimination Mechanism | Not a primary waste elimination process. | Primary mechanism for eliminating waste products from the body. |
| Efflux Pumps and Transporters Involved | Few efflux pumps and transporters involved. | Numerous efflux pumps and transporters involved in active transport. |
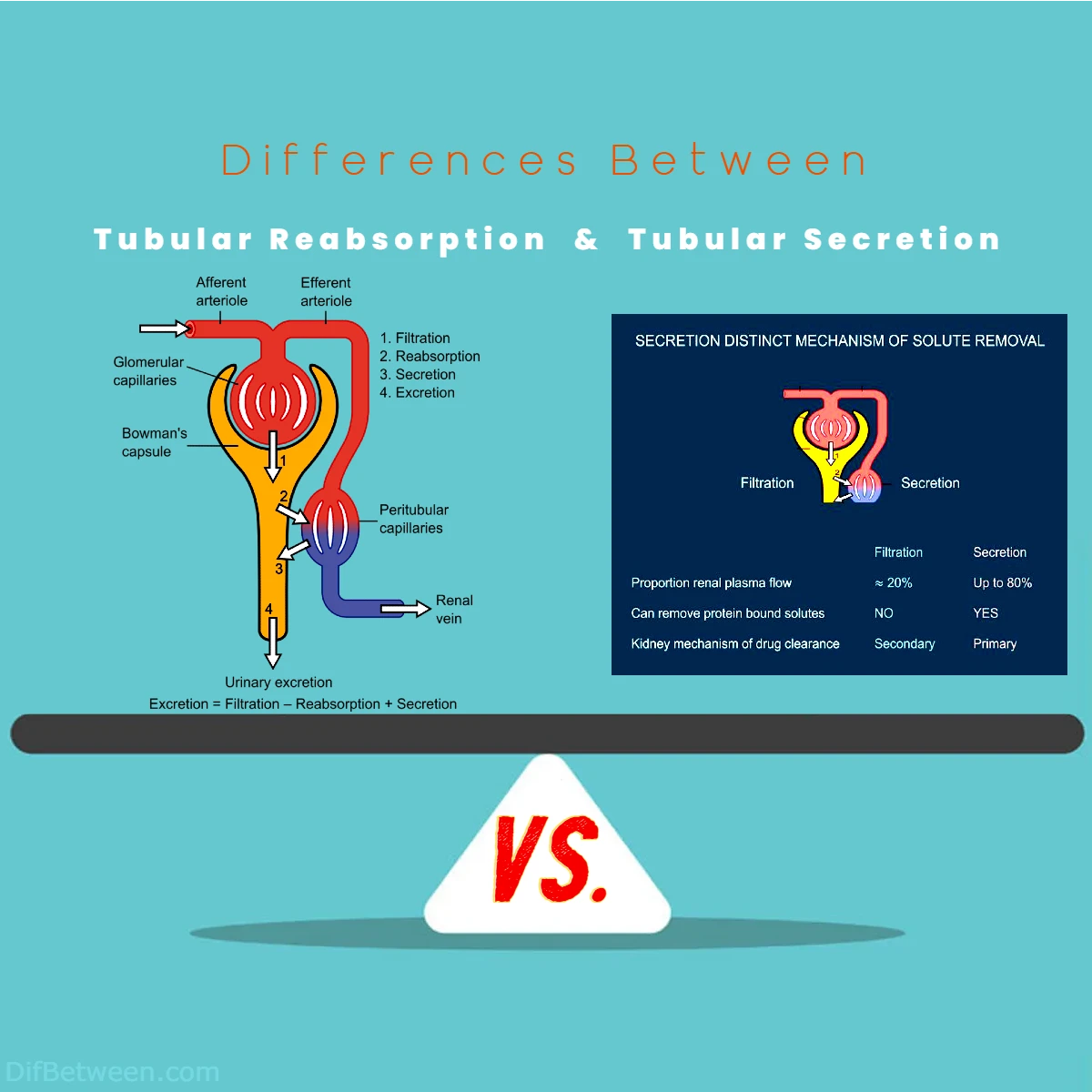
Picture this: deep within your kidneys, a fascinating battle unfolds daily, involving two remarkable processes—tubular reabsorption and tubular secretion. It’s a tale of intricate molecular ballet, where substances are selectively retained or actively expelled, all in the name of maintaining your body’s delicate balance.
Differences Between Tubular Reabsorption and Tubular Secretion
Tubular reabsorption and tubular secretion are two vital processes in renal physiology. The main differences between them lie in their actions and roles within the kidney’s nephrons. Tubular reabsorption involves the selective reclamation of essential substances, such as water, glucose, and ions, from the initial filtrate back into the bloodstream, maintaining the body’s homeostasis. In contrast, tubular secretion actively transports waste products, like hydrogen ions, creatinine, and drugs, from the bloodstream into the renal tubules, crucial for detoxification and pH regulation. These processes work in harmony, ensuring that the body retains what it needs and efficiently eliminates what it doesn’t, playing a pivotal role in overall health.
The Basics
Tubular Reabsorption
Tubular reabsorption is the process by which the renal tubules selectively reclaim essential substances from the ultrafiltrate (the initial filtrate produced by the glomerulus) back into the bloodstream. This reclamation is crucial because not all substances in the ultrafiltrate should be excreted in urine; some need to be retained to maintain the body’s homeostasis.
During tubular reabsorption, the renal tubules reabsorb substances like water, glucose, amino acids, ions (e.g., sodium, potassium, calcium, and chloride), and other essential solutes from the ultrafiltrate. These substances pass through the tubular epithelial cells lining the nephron and return to the bloodstream through peritubular capillaries. As a result, the composition of the fluid in the renal tubules changes, with the reabsorption of valuable molecules, making it more concentrated.
Tubular Secretion
Conversely, tubular secretion is the process by which the renal tubules actively transport certain substances from the bloodstream into the renal tubules. This secretion allows the removal of waste products, excess ions, and toxins from the body while also controlling the body’s acid-base balance and electrolyte levels.
During tubular secretion, specific substances such as hydrogen ions (H+), creatinine, drugs, and metabolic waste products are actively transported from the peritubular capillaries into the renal tubules. This selective transport plays a critical role in eliminating unwanted or harmful substances from the body, preventing their accumulation in the bloodstream.
Now that we have a basic understanding of these processes, let’s delve deeper into the key differences between tubular reabsorption and tubular secretion.
Mechanisms of Action
Tubular Reabsorption Mechanism
Tubular reabsorption primarily occurs through passive and active transport mechanisms in the renal tubules. Here’s a breakdown of the key mechanisms involved:
1. Passive Diffusion
Passive diffusion is a vital mechanism for the reabsorption of lipid-soluble substances like oxygen, carbon dioxide, and lipid-soluble drugs. These molecules can easily pass through the lipid bilayer of the tubular epithelial cells due to their hydrophobic nature.
2. Active Transport
Active transport mechanisms are responsible for reabsorbing ions and polar molecules, such as glucose and amino acids. The sodium-potassium pump (Na+/K+ pump) is a prime example of an active transport system in tubular reabsorption. This pump actively transports sodium ions out of the tubular epithelial cells into the interstitial fluid, creating a sodium concentration gradient that drives the reabsorption of other solutes like glucose and amino acids.
3. Facilitated Diffusion
Facilitated diffusion occurs when carrier proteins in the tubular epithelial cells assist in the reabsorption of certain molecules. An example is the reabsorption of glucose through glucose transporters (GLUTs). These transporters facilitate the movement of glucose from the tubular lumen into the epithelial cells, and from there, it enters the bloodstream via facilitated diffusion.
Tubular Secretion Mechanism
Tubular secretion, on the other hand, primarily involves active transport mechanisms for the movement of substances from the blood into the tubular lumen. Here are the key mechanisms at play:
1. Active Transport
Similar to tubular reabsorption, active transport is crucial in tubular secretion. Proximal tubular cells actively secrete hydrogen ions (H+) into the tubular lumen to regulate blood pH. Additionally, organic anions and cations, such as creatinine and some drugs, are actively transported into the tubules for excretion.
2. Counter-Transport
Counter-transport, also known as antiport, is a mechanism where one substance is actively transported in one direction while another is transported in the opposite direction. For example, the exchange of hydrogen ions (H+) for bicarbonate ions (HCO3-) in the proximal tubules helps regulate blood pH.
3. Passive Diffusion
While active transport is the predominant mechanism in tubular secretion, some substances may also undergo passive diffusion from the peritubular capillaries into the tubular lumen. However, this is less common compared to active transport.
Selectivity
Tubular Reabsorption Selectivity
Tubular reabsorption is highly selective, ensuring that essential substances are retained in the body while unnecessary waste is excreted. Here’s what typically gets reabsorbed:
1. Water
Water reabsorption occurs in various segments of the renal tubules, primarily in the proximal tubules and the descending limb of the loop of Henle. The reabsorption of water is tightly regulated to maintain body fluid balance.
2. Glucose and Amino Acids
The proximal tubules are responsible for reabsorbing nearly all filtered glucose and amino acids. This process is highly efficient and prevents the loss of these essential nutrients in urine.
3. Ions
Sodium ions (Na+) are actively reabsorbed throughout the renal tubules, primarily in the proximal tubules. This reabsorption sets the stage for the reabsorption of other ions like chloride (Cl-), potassium (K+), and calcium (Ca2+).
4. Other Solutes
Various solutes, including bicarbonate ions (HCO3-), phosphate ions (HPO4^2-), and sulfate ions (SO4^2-), are reabsorbed in specific segments of the renal tubules to maintain electrolyte balance.
Tubular Secretion Selectivity
Tubular secretion is selective but focuses on removing waste products and regulating pH and electrolyte balance. Here’s what typically gets secreted:
1. Hydrogen Ions (H+)
The secretion of hydrogen ions into the tubular lumen helps regulate blood pH by eliminating excess acidity.
2. Creatinine
Creatinine, a metabolic waste product, is actively secreted into the tubules. It serves as a marker of renal function and is typically excreted in urine.
3. Drugs and Toxins
Many drugs, toxins, and metabolic byproducts are actively secreted into the renal tubules for elimination from the body. This is a crucial mechanism for detoxification.
4. Potassium Ions (K+)
Potassium ions are also subject to secretion in the distal tubules and collecting ducts to regulate blood potassium levels.
Location
Tubular Reabsorption Location
Tubular reabsorption occurs in various segments of the renal tubules, with each segment specializing in reabsorbing specific substances:
1. Proximal Tubules
The proximal tubules are the primary site of reabsorption for glucose, amino acids, sodium ions, water, and various other solutes. They reabsorb approximately 60-70% of the filtered load.
2. Loop of Henle
The descending limb of the loop of Henle is crucial for water reabsorption, while the ascending limb is responsible for reabsorbing sodium and chloride ions.
3. Distal Tubules and Collecting Ducts
The distal tubules and collecting ducts fine-tune the reabsorption of sodium, potassium, and water based on the body’s needs and hormonal signals.
Tubular Secretion Location
Tubular secretion primarily occurs in the proximal tubules and, to a lesser extent, in the distal tubules and collecting ducts:
1. Proximal Tubules
The proximal tubules play a significant role in the active secretion of hydrogen ions (H+) to regulate blood pH and the secretion of organic anions and cations, including creatinine and some drugs.
2. Distal Tubules and Collecting Ducts
In the distal tubules and collecting ducts, additional secretion of potassium ions (K+) and hydrogen ions (H+) occurs to maintain electrolyte and acid-base balance.
Regulatory Factors: Hormones and Control
Tubular Reabsorption Regulation
The reabsorption of substances in the renal tubules, particularly sodium ions and water, is tightly regulated by various hormones and physiological factors:
1. Antidiuretic Hormone (ADH)
ADH, also known as vasopressin, plays a crucial role in regulating water reabsorption. It increases the permeability of the distal tubules and collecting ducts to water, allowing for greater reabsorption when the body needs to conserve water.
2. Aldosterone
Aldosterone is a hormone that regulates sodium reabsorption in the distal tubules and collecting ducts. It promotes sodium reabsorption and potassium secretion, helping to maintain blood pressure and electrolyte balance.
3. Atrial Natriuretic Peptide (ANP)
ANP is released by the heart in response to increased blood volume and pressure. It inhibits sodium reabsorption in the distal tubules and collecting ducts, promoting sodium excretion and reducing blood volume and pressure.
4. Parathyroid Hormone (PTH)
PTH regulates calcium reabsorption in the renal tubules. It increases calcium reabsorption in the distal tubules, helping to maintain calcium balance in the body.
Tubular Secretion Regulation
Tubular secretion is also under the influence of various hormones and regulatory factors:
1. Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS system plays a crucial role in regulating blood pressure and sodium reabsorption. Renin, an enzyme released by the kidneys, initiates the formation of angiotensin II, which stimulates aldosterone release. Aldosterone, in turn, enhances sodium reabsorption and potassium secretion in the distal tubules.
2. Acid-Base Balance
The secretion of hydrogen ions (H+) in the proximal tubules is regulated to maintain blood pH within a narrow range. Acidosis (low blood pH) triggers increased H+ secretion, while alkalosis (high blood pH) reduces H+ secretion.
3. Diuretics
Certain medications called diuretics can influence tubular secretion by inhibiting sodium reabsorption. These drugs are often prescribed to manage conditions like hypertension and edema.
Clinical Significance
Tubular Reabsorption and Health
Understanding tubular reabsorption is critical in assessing and managing various health conditions:
1. Diabetes Mellitus
In diabetes mellitus, the reabsorption of glucose in the renal tubules is impaired due to high blood glucose levels. This leads to glucose spillage into the urine, a condition known as glycosuria. Monitoring glycosuria is crucial for diabetes management.
2. Hypertension
Alterations in sodium reabsorption can contribute to hypertension (high blood pressure). Abnormalities in the renin-angiotensin-aldosterone system, which regulates sodium reabsorption, can play a role in hypertension development.
3. Edema
Edema, the accumulation of excess fluid in body tissues, can occur when there’s a disruption in the reabsorption of water in the renal tubules. Diuretics, which promote water excretion, are often prescribed to manage edema.
Tubular Secretion and Health
Tubular secretion is equally significant in understanding and managing health conditions:
1. Kidney Function Assessment
Creatinine clearance, a measure of how efficiently the kidneys clear creatinine from the blood, is used to assess kidney function. Reduced tubular secretion of creatinine can indicate impaired kidney function.
2. Acid-Base Balance Disorders
Tubular secretion of hydrogen ions (H+) is vital for maintaining blood pH. Disorders like renal tubular acidosis (RTA) can disrupt this process, leading to acid-base imbalances.
3. Drug Excretion
Understanding tubular secretion is crucial for pharmacology. Drugs that are actively secreted into the renal tubules are more efficiently eliminated from the body. This knowledge guides medication dosing and administration.
Comparative Table: Tubular Reabsorption vs. Tubular Secretion
Let’s summarize the key differences between tubular reabsorption and tubular secretion in a comparative table:
| Aspect | Tubular Reabsorption | Tubular Secretion |
|---|---|---|
| Definition | Reclaiming essential substances from ultrafiltrate. | Actively transporting certain substances into tubules. |
| Mechanisms | Passive diffusion, active transport, facilitated diffusion. | Active transport, counter-transport, passive diffusion. |
| Selectivity | Highly selective, retains essential substances. | Selective, focuses on waste removal and pH regulation. |
| Location | Proximal tubules, loop of Henle, distal tubules, collecting ducts. | Proximal tubules, distal tubules, collecting ducts. |
| Regulatory Factors | ADH, aldosterone, ANP, PTH regulate reabsorption. | RAAS, acid-base balance, diuretics affect secretion. |
| Clinical Significance | Impacts diabetes, hypertension, and edema. | Assess kidney function, manage acid-base imbalances, and drug excretion. |
Common Misconceptions
1. Reabsorption Equals 100%
It’s important to note that not all substances are reabsorbed completely. Some are intentionally excreted in urine. For instance, waste products like urea and creatinine are only partially reabsorbed.
2. Tubular Secretion Is Only About Waste
While tubular secretion is crucial for eliminating waste products, it also plays a vital role in regulating blood pH, excreting drugs and toxins, and controlling electrolyte balance.
3. Reabsorption and Secretion Are Separate Processes
In reality, reabsorption and secretion often work together in the same nephron to maintain overall homeostasis. For example, while sodium ions are reabsorbed in the proximal tubule, they can also be secreted in the distal tubule.
In Conclusion
Tubular reabsorption and tubular secretion are intricate processes that take place within the nephrons of the kidney. Together, they help maintain the body’s internal balance by reabsorbing vital substances and eliminating waste products. These processes are tightly regulated by hormones and play a crucial role in various health conditions, making them a subject of great interest in the fields of nephrology and pharmacology.
As we wrap up our exploration, it’s worth acknowledging the remarkable complexity of the human body and its ability to meticulously regulate the composition of bodily fluids. Tubular reabsorption and tubular secretion are just two chapters in the epic saga of renal physiology, but they are chapters of utmost importance in the ongoing story of human health and well-being.
FAQs
Tubular reabsorption is a renal process that involves the selective reclamation of essential substances, such as water, glucose, and ions, from the initial filtrate back into the bloodstream within the renal tubules. Tubular secretion, on the other hand, is the active transport of waste products, like hydrogen ions, creatinine, and drugs, from the bloodstream into the renal tubules for elimination. The key difference lies in their actions: reabsorption retains valuable substances, while secretion eliminates waste.
Tubular reabsorption occurs in various segments of the renal tubules, including the proximal tubules, loop of Henle, distal tubules, and collecting ducts. Tubular secretion primarily takes place in the proximal tubules, with some additional secretion occurring in the distal tubules and collecting ducts.
Tubular reabsorption is regulated by hormones like ADH (antidiuretic hormone), aldosterone, ANP (atrial natriuretic peptide), and PTH (parathyroid hormone), which influence the reabsorption of specific substances. Tubular secretion is influenced by the renin-angiotensin-aldosterone system (RAAS), acid-base balance hormones, and certain medications like diuretics.
Tubular reabsorption and secretion play crucial roles in assessing kidney function and managing various health conditions. Tubular reabsorption impacts diabetes, hypertension, and fluid balance, while tubular secretion is essential for eliminating waste, regulating pH, and managing drug elimination.
Tubular reabsorption and tubular secretion are interdependent processes that work in harmony within the nephrons to maintain overall homeostasis. They complement each other to ensure the body retains essential substances while efficiently eliminating waste, playing a pivotal role in overall health and balance.
Read More:
Contents