| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Presence of Cell Wall | Absent | Present |
| Cell Wall Composition | None | Atypical (lacks peptidoglycan) |
| Genome Size | Small | Larger |
| Genome Complexity | Minimal | Complex |
| Nutritional Requirements | Fastidious | Exploits host cellular machinery |
| Reliance on Host for Nutrients | Yes | Yes |
| Tissue Preference | Mucous membranes, respiratory, urogenital | Urogenital, ocular, respiratory (in birds) |
| Associated Diseases | Respiratory infections, urogenital conditions | Chlamydia, trachoma, zoonotic infections |
| Reproductive Strategy | Binary fission | Alternation between elementary and reticulate bodies |
| Host Adhesion | Adhesion to host cells | Intracellular lifestyle |
| Intracellular Growth | No | Yes |
| Immune Evasion | Limited | Effective |
| Diagnostic Challenges | Lack of cell wall, asymptomatic infections | Asymptomatic infections, need for routine screening |
| Treatment Challenges | Antibiotic resistance | Risk of antibiotic resistance, early treatment critical |
| Public Health Impact | Outbreaks in various settings, respiratory infections | Leading cause of STIs, potential for severe complications |
| Research and Future Directions | Antibiotic resistance, Mycoplasma genomics, Host-Pathogen Interactions | Antibiotic resistance, Vaccine Development, Molecular Mechanisms |
Mycoplasma, the minimalist microbes, are known for their unique lifestyle, marked by the absence of a cell wall and a minimalistic genome. On the other hand, Chlamydia, the intracellular invaders, thrive by hijacking host cells and leading an obligate intracellular life. With their dissimilar reproductive strategies and roles in diseases, these microorganisms paint a vivid picture of the wonders and complexities of the microbial world.
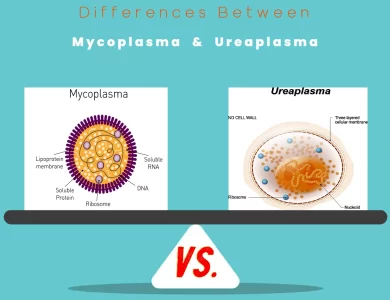
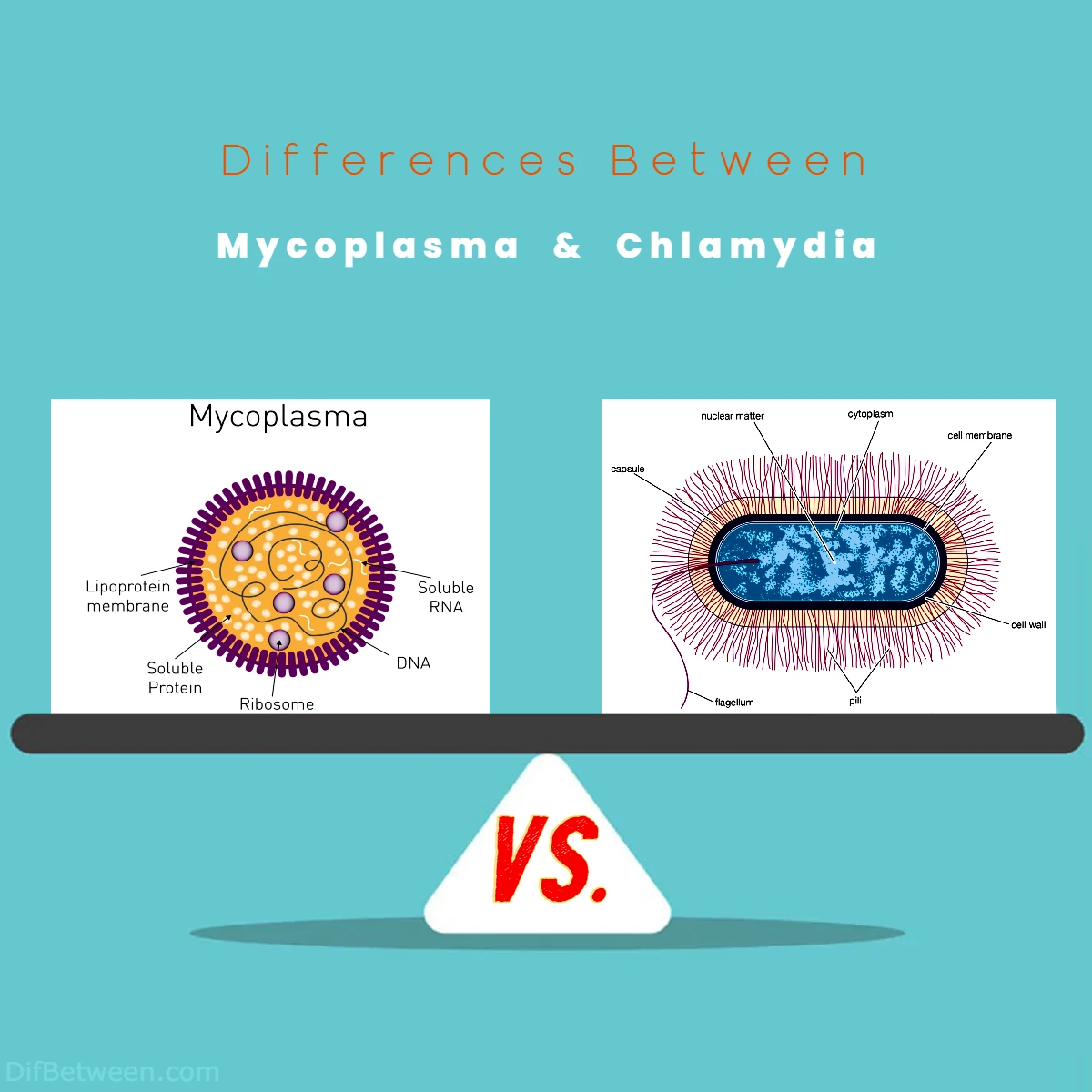
Differences Between Mycoplasma and Chlamydia
The primary distinctions between Mycoplasma and Chlamydia revolve around their cellular characteristics, lifestyles, and impact on health. Mycoplasma stands out with its lack of a cell wall, resulting in flexibility in shape and unique genome minimalism. In contrast, Chlamydia possesses an atypical cell wall and an obligate intracellular lifestyle, living within host cells. These differences influence their diagnostic challenges, treatment strategies, and public health implications. Understanding these variations is essential for healthcare professionals and curious minds alike.
The Basics
Mycoplasma: The Minimalists of the Microbial World
Mycoplasma is a genus of bacteria characterized by their unique features and lifestyle. One of the most remarkable aspects of Mycoplasma is their minimalistic approach to life. These bacteria have one of the smallest genomes among free-living organisms, containing only the essential genes for survival. As a result, they lack a cell wall, which is a defining characteristic of most bacteria. This absence of a cell wall allows them to take on various shapes, from round to filamentous, making them quite adaptable in their environment.
Key Characteristics of Mycoplasma
To better understand Mycoplasma, let’s take a closer look at their key characteristics:
Lack of Cell Wall
The absence of a cell wall is a defining feature of Mycoplasma. This unique trait not only makes them highly flexible in terms of shape but also poses challenges in their identification and treatment.
Minimal Genome
Mycoplasma has one of the smallest genomes among all cellular life forms. This minimalism is due to their reliance on a host organism for many essential nutrients, which has led to the loss of numerous non-essential genes.
Fastidious Nutritional Requirements
Mycoplasma are known to be fastidious in their nutritional requirements, which means they have specific and often complex needs for growth and replication. They are reliant on external sources for crucial nutrients, which can make them challenging to culture and study.
Predilection for Mucous Membranes
These microorganisms often have a preference for mucous membranes in humans and animals. They can colonize various host tissues, causing infections in the respiratory and urogenital tracts.
Role in Diseases
Mycoplasma species are associated with a range of diseases in humans and animals. Some notable examples include Mycoplasma pneumoniae, which causes respiratory infections, and Mycoplasma genitalium, which is linked to urogenital conditions.
Chlamydia: The Intracellular Invaders
Chlamydia, on the other hand, is a different class of microorganism. They belong to a group of bacteria known as Chlamydiae, and like Mycoplasma, they have some distinctive traits. One of the most notable features of Chlamydia is their intracellular lifestyle. These bacteria live within the cells of their host, making them obligate intracellular parasites.
Key Characteristics of Chlamydia
Let’s explore the key characteristics that define Chlamydia:
Obligate Intracellular Parasites
Chlamydia are obligate intracellular parasites, which means they cannot survive or replicate outside of host cells. They have evolved complex mechanisms to invade and manipulate host cells, allowing them to thrive within the cellular environment.
Unique Reproductive Cycle
Chlamydia possess a unique reproductive cycle involving two distinct forms: the elementary body (EB) and the reticulate body (RB). The EB is the infectious form, while the RB is responsible for replication within host cells.
Human and Animal Pathogens
Chlamydia can infect both humans and animals, causing a variety of diseases. Chlamydia trachomatis, for example, is a leading cause of sexually transmitted infections (STIs), while Chlamydia psittaci can infect birds and occasionally humans, causing zoonotic infections.
Silent Infections
One striking aspect of Chlamydia infections is that they can often be asymptomatic, especially in the early stages. This makes early detection and treatment critical to prevent complications.
Involvement in Health Issues
Chlamydia infections can lead to various health problems, such as genital and ocular infections in humans and respiratory diseases in birds. Untreated Chlamydia infections may result in severe complications.
Now that we’ve acquainted ourselves with the fundamental characteristics of Mycoplasma and Chlamydia, let’s dive deeper into the differences between these two fascinating microorganisms.
Cell Wall Presence
One of the most striking differences between Mycoplasma and Chlamydia is the presence or absence of a cell wall.
Mycoplasma: These bacteria are well-known for their lack of a cell wall. This unique feature makes them highly flexible in terms of shape and structure. The absence of a cell wall also poses challenges in terms of identification and treatment, as many common antibiotics target cell wall synthesis. Mycoplasma’s lack of a cell wall is considered an evolutionary adaptation, allowing them to colonize a variety of host tissues and evade the immune system more effectively.
Chlamydia: In contrast, Chlamydia bacteria possess a cell wall, albeit a somewhat atypical one. The Chlamydia cell wall is structurally different from that of most bacteria and lacks peptidoglycan, a common component of bacterial cell walls. This unique cell wall is believed to play a role in their ability to live within host cells.
Table 1: Cell Wall Presence in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Presence of Cell Wall | Absent | Present |
| Cell Wall Composition | None | Atypical |
Genome Size and Complexity
The genomes of Mycoplasma and Chlamydia exhibit significant differences in terms of size and complexity.
Mycoplasma: Mycoplasma has one of the smallest genomes among all cellular life forms. Their minimalistic approach to genome size is a result of their reliance on a host organism for many essential nutrients. Over time, they have shed non-essential genes, resulting in a streamlined genome. This minimal genome size is a remarkable feature of Mycoplasma.
Chlamydia: Chlamydia, while still considered intracellular parasites, have relatively larger genomes compared to Mycoplasma. Their genomes are more complex and contain a wider range of genes. This complexity is likely related to their unique reproductive cycle and intracellular lifestyle, which involves complex interactions with host cells.
Table 2: Genome Size and Complexity in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Genome Size | Small | Larger |
| Genome Complexity | Minimal | Complex |
Nutritional Requirements
Both Mycoplasma and Chlamydia have specific nutritional requirements, but their approaches to obtaining these nutrients differ.
Mycoplasma: Mycoplasma are known to be fastidious in their nutritional requirements. They have specific and often complex needs for growth and replication. Unlike most bacteria, Mycoplasma cannot synthesize many essential nutrients on their own. Instead, they rely on external sources, such as host cells or specialized culture media, for these nutrients. This makes Mycoplasma challenging to culture and study in the laboratory.
Chlamydia: Chlamydia, while also having specific nutritional requirements, have evolved unique strategies to acquire these nutrients. As obligate intracellular parasites, they manipulate host cells to extract the necessary nutrients for their survival and replication. Chlamydia’s ability to hijack host cellular machinery is a key factor in their intracellular lifestyle.
Table 3: Nutritional Requirements in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Nutritional Requirements | Fastidious | Exploits host cellular machinery |
| Reliance on Host for Nutrients | Yes | Yes |
Tissue Preference and Diseases
Both Mycoplasma and Chlamydia can cause a range of diseases in humans and animals, with a preference for specific tissues.
Mycoplasma: Mycoplasma species often have a predilection for mucous membranes in humans and animals. They can colonize various host tissues, leading to infections in the respiratory and urogenital tracts. Mycoplasma pneumoniae, for example, is a common cause of respiratory infections, while Mycoplasma genitalium is associated with urogenital conditions.
Chlamydia: Chlamydia bacteria also infect humans and animals, but their tissue preferences and associated diseases differ. Chlamydia trachomatis primarily infects the urogenital and ocular tissues in humans, leading to conditions such as chlamydia and trachoma. Chlamydia psittaci, on the other hand, is known to infect birds and can occasionally be transmitted to humans, causing zoonotic infections.
Table 4: Tissue Preference and Associated Diseases in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Tissue Preference | Mucous membranes, respiratory, urogenital | Urogenital, ocular, respiratory (in birds) |
| Associated Diseases | Respiratory infections, urogenital conditions | Chlamydia, trachoma, zoonotic infections |
Reproductive Strategies
The reproductive strategies of Mycoplasma and Chlamydia also exhibit notable differences.
Mycoplasma: Mycoplasma reproduce through binary fission, a process in which a single cell splits into two identical daughter cells. This is a common method of reproduction in bacteria and results in the growth of bacterial populations.
Chlamydia: Chlamydia possess a unique and complex reproductive cycle. They alternate between two distinct forms: the elementary body (EB) and the reticulate body (RB). The EB is the infectious form that can survive outside of host cells, while the RB is responsible for replication within host cells. This alternation between forms is a crucial aspect of Chlamydia’s ability to infect and thrive within host tissues.
Table 5: Reproductive Strategies in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Reproductive Strategy | Binary fission | Alternation between elementary and reticulate bodies |
Host Interaction and Pathogenesis
Both Mycoplasma and Chlamydia interact with their host organisms in unique ways, contributing to their pathogenesis.
Mycoplasma: Mycoplasma’s pathogenicity often involves the adhesion of these bacteria to host cells. They may produce adhesins that enable them to attach to host cell surfaces, which can lead to infections and tissue damage. Mycoplasma pneumoniae, for example, attaches to the respiratory epithelium, causing respiratory infections.
Chlamydia: Chlamydia’s pathogenesis is closely tied to their intracellular lifestyle. They enter host cells, where they can replicate and evade the immune system. Chlamydia’s ability to manipulate host cell functions and acquire nutrients is key to their success as pathogens.
Table 6: Host Interaction and Pathogenesis in Mycoplasma and Chlamydia
| Characteristic | Mycoplasma | Chlamydia |
|---|---|---|
| Host Adhesion | Adhesion to host cells | Intracellular lifestyle |
| Intracellular Growth | No | Yes |
| Immune Evasion | Limited | Effective |
Clinical Impact
The clinical impact of Mycoplasma and Chlamydia infections varies, with both having significant implications for public health.
Mycoplasma: Mycoplasma infections can result in a range of clinical conditions, including respiratory infections like atypical pneumonia caused by Mycoplasma pneumoniae. Some Mycoplasma species are also implicated in urogenital infections. The impact of Mycoplasma infections on public health is significant, with the potential for outbreaks in communities.
Chlamydia: Chlamydia infections, particularly those caused by Chlamydia trachomatis, are a major public health concern. They are a leading cause of sexually transmitted infections (STIs) and can lead to serious complications if left untreated. Chlamydia infections are often asymptomatic, which further underscores the importance of regular screening and early detection.
Table 7: Clinical Impact of Mycoplasma and Chlamydia Infections
| Characteristic | Mycoplasma Infections | Chlamydia Infections |
|---|---|---|
| Clinical Impact | Respiratory and urogenital infections | Leading cause of STIs with potential for complications |
Diagnostic Challenges
Mycoplasma:
Diagnosing Mycoplasma infections can be challenging due to several factors. The lack of a cell wall in Mycoplasma bacteria means that traditional Gram staining techniques, which rely on the presence of a cell wall, cannot be used. Instead, specialized staining methods, such as the use of fluorescent dyes and molecular techniques like polymerase chain reaction (PCR), are often required for accurate diagnosis. Additionally, Mycoplasma infections can be asymptomatic or present with mild symptoms, further complicating diagnosis.
Chlamydia:
Chlamydia diagnosis also presents unique challenges. Many Chlamydia infections, especially in the early stages, are asymptomatic. As a result, individuals may be unaware that they are infected. To address this, routine screening is recommended for sexually active individuals to detect and treat Chlamydia infections before they lead to complications. Nucleic acid amplification tests (NAATs) are the gold standard for Chlamydia diagnosis, providing high sensitivity and specificity.
Table 8: Diagnostic Challenges in Mycoplasma and Chlamydia Infections
| Characteristic | Mycoplasma Diagnosis | Chlamydia Diagnosis |
|---|---|---|
| Diagnostic Challenges | Lack of cell wall, asymptomatic infections | Asymptomatic infections, need for routine screening |
Treatment Strategies
Mycoplasma:
Treating Mycoplasma infections typically involves the use of antibiotics, but there are specific challenges. Mycoplasma bacteria are resistant to many common antibiotics that target cell wall synthesis due to their lack of a cell wall. Therefore, antibiotics that act on other bacterial processes, such as protein synthesis, are usually employed. Tetracyclines, macrolides, and fluoroquinolones are commonly used to treat Mycoplasma infections. However, antibiotic resistance in Mycoplasma species is a growing concern, necessitating careful selection of appropriate antibiotics.
Chlamydia:
Chlamydia infections are also treated with antibiotics, and early treatment is crucial to prevent complications. The antibiotics of choice for Chlamydia trachomatis infections are typically azithromycin or doxycycline. These antibiotics are highly effective when administered as recommended. However, antibiotic resistance in Chlamydia has been reported in some cases, emphasizing the importance of adherence to treatment guidelines.
Table 9: Treatment Strategies for Mycoplasma and Chlamydia Infections
| Characteristic | Mycoplasma Treatment | Chlamydia Treatment |
|---|---|---|
| Treatment Challenges | Antibiotic resistance | Risk of antibiotic resistance, early treatment critical |
Public Health Impact
Mycoplasma:
Mycoplasma infections, while not as widely recognized as Chlamydia, can have a significant public health impact. Mycoplasma pneumoniae, in particular, is a common cause of respiratory infections, including atypical pneumonia. These infections can lead to hospitalizations and can affect people of all age groups. Outbreaks of Mycoplasma infections have been reported in various settings, such as schools and healthcare facilities.
Chlamydia:
Chlamydia has a substantial impact on public health. It is one of the most commonly reported sexually transmitted infections (STIs) globally. The consequences of untreated Chlamydia infections can be severe, leading to pelvic inflammatory disease (PID), infertility, ectopic pregnancy, and an increased risk of HIV transmission. Chlamydia prevention efforts include regular screening, safe sexual practices, and timely treatment.
Table 10: Public Health Impact of Mycoplasma and Chlamydia Infections
| Characteristic | Mycoplasma Impact on Public Health | Chlamydia Impact on Public Health |
|---|---|---|
| Public Health Impact | Outbreaks in various settings, respiratory infections | Leading cause of STIs, potential for severe complications |
Research and Future Directions
While much is known about Mycoplasma and Chlamydia, ongoing research continues to reveal new insights into these microorganisms. Some areas of research interest include:
Mycoplasma:
- Antibiotic Resistance: Understanding the mechanisms of antibiotic resistance in Mycoplasma and developing alternative treatment strategies.
- Mycoplasma Genomics: Investigating the genomic evolution of Mycoplasma species and the factors driving their minimalistic genomes.
- Host-Pathogen Interactions: Studying how Mycoplasma bacteria interact with host cells and tissues to cause disease.
Chlamydia:
- Antibiotic Resistance: Monitoring and addressing antibiotic resistance in Chlamydia trachomatis to ensure effective treatment.
- Vaccine Development: Ongoing efforts to develop a vaccine against Chlamydia to prevent infections and their complications.
- Molecular Mechanisms: Research into the molecular mechanisms that allow Chlamydia to manipulate host cells and evade the immune system.
Conclusion
In our exploration of the microbial world, we’ve delved into the intriguing differences between Mycoplasma and Chlamydia. These two genera of microorganisms, though both responsible for diseases in humans and animals, have distinct characteristics and lifestyles that set them apart. From their approach to cell walls and genome size to their reproductive strategies and clinical impact, Mycoplasma and Chlamydia showcase the fascinating diversity of microorganisms.
Understanding these differences is not only of scientific interest but also essential for healthcare professionals, researchers, and the general public. It highlights the need for accurate diagnostic methods, effective treatments, and preventive measures to combat the diseases caused by these microorganisms. As we continue to expand our knowledge of the microbial world, we gain valuable insights that can lead to better healthcare and a deeper appreciation of the complex interactions between microorganisms and their hosts.
FAQs
Mycoplasma and Chlamydia are two different genera of microorganisms. Mycoplasma are bacteria known for their lack of a cell wall, while Chlamydia are bacteria with an atypical cell wall.
Mycoplasma lack a cell wall, which makes them highly adaptable in terms of shape. In contrast, Chlamydia possess an atypical cell wall.
The absence of a cell wall in Mycoplasma poses challenges in terms of identification and treatment, as many antibiotics target cell wall synthesis. Chlamydia’s atypical cell wall is related to its ability to live within host cells.
Mycoplasma have one of the smallest genomes among cellular life forms, while Chlamydia have relatively larger and more complex genomes.
Mycoplasma are fastidious and have specific nutritional requirements, relying on external sources for essential nutrients. Chlamydia, as intracellular parasites, exploit host cellular machinery for nutrients.
Mycoplasma often colonize mucous membranes, respiratory, and urogenital tissues. Chlamydia primarily infect urogenital and ocular tissues in humans and respiratory tissues in birds.
Mycoplasma can cause respiratory infections and urogenital conditions, while Chlamydia is a leading cause of sexually transmitted infections (STIs) and can lead to various complications.
Mycoplasma reproduce through binary fission, while Chlamydia alternates between elementary and reticulate bodies for replication within host cells.
Diagnosing Mycoplasma infections can be challenging due to their lack of a cell wall, while Chlamydia infections are often asymptomatic. Both require specific diagnostic methods. Mycoplasma may develop antibiotic resistance, and early treatment is crucial for Chlamydia.
Mycoplasma infections can lead to outbreaks in various settings and respiratory infections, while Chlamydia is a major public health concern, being a leading cause of STIs with potential for severe complications.
Read More: