| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Cell Wall | Absent (lack a peptidoglycan cell wall) | Absent (lack a peptidoglycan cell wall) |
| Size | 0.2 to 0.8 µm (small) | 0.15 to 0.3 µm (small) |
| Motility | Exhibits gliding and twitching motility | – |
| Reproduction | Binary fission | Binary fission |
| Urea Metabolism | Cannot metabolize urea | Metabolizes urea, produces ammonia |
| Colonization | Versatile, found in soil, plants, animals | Primarily colonizes the urogenital tract |
| Pathogenicity | Some species can cause human and animal diseases | Some strains associated with urinary and reproductive diseases |
| Diagnosis | PCR, serological tests, culture-based techniques | PCR, serological tests, culture-based techniques |
| Treatment | Antibiotics (tetracyclines, macrolides, fluoroquinolones) | Antibiotics (tetracyclines, macrolides) |
| Antibiotic Resistance | Growing concern | Variability in susceptibility patterns |
| Genetic Diversity | Varies in gene content and organization | Genetic diversity influences host specificity |
| Evolutionary History | Adaptation to parasitic lifestyles, loss of cell wall | Likely adaptation to urogenital tract, urea metabolism |
| Environmental Resilience | Flexibility in host colonization, sensitivity to environmental changes | Adaptability to host environments, sensitivity to environmental changes |
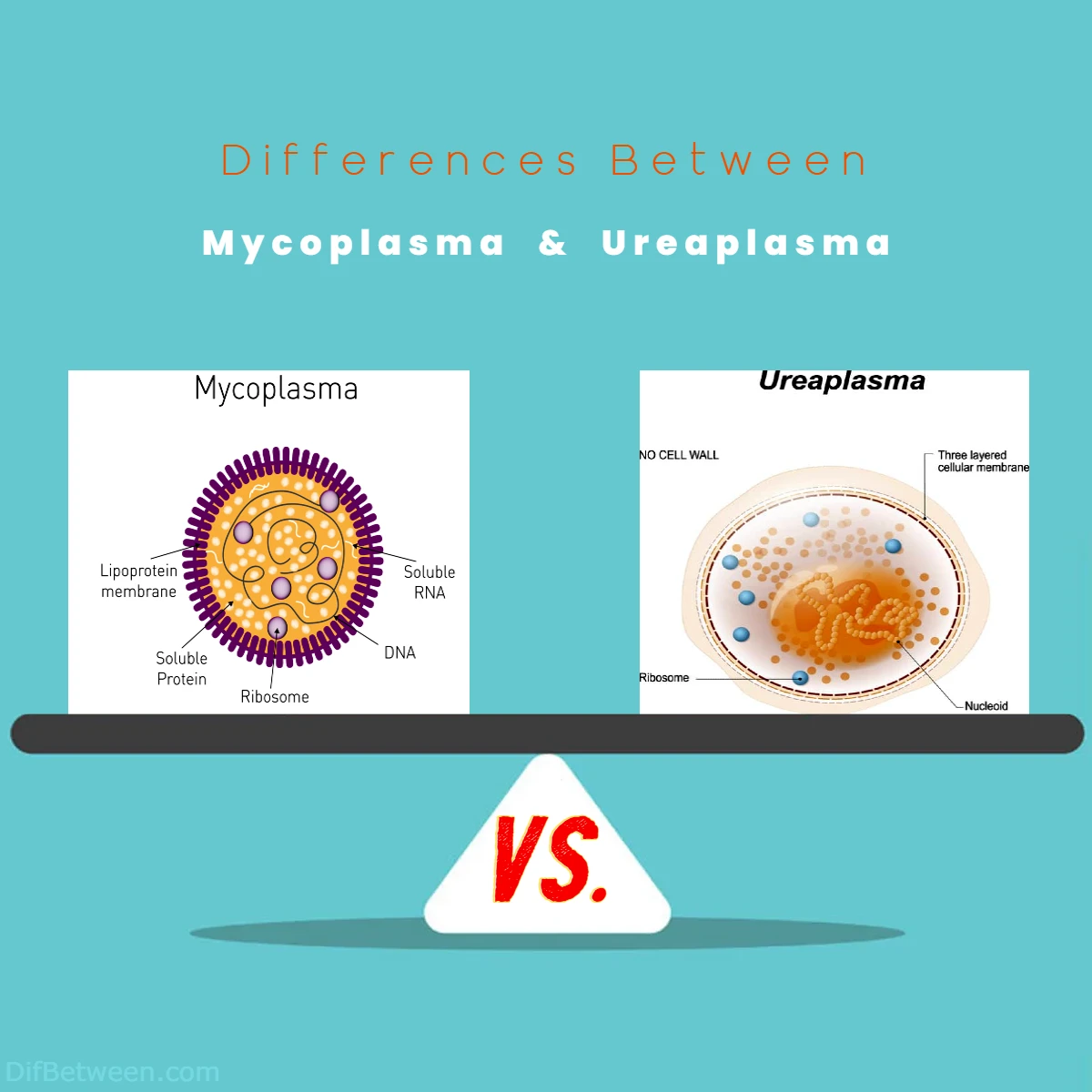
Mycoplasma, often dubbed as “nature’s minimalists,” and Ureaplasma, the urea utilizers, may share some striking resemblances, but it’s the subtle distinctions that make them stand out. From their unique cell wall structures (or the lack thereof) to their ecological niches and impact on human health, there’s a world of discovery waiting for us.
Differences Between Mycoplasma and Ureaplasma
The main differences between Mycoplasma and Ureaplasma lie in their cell wall structures, size, metabolic capabilities, and ecological niches. Mycoplasma lacks a peptidoglycan cell wall, while Ureaplasma shares this characteristic. Mycoplasma is slightly larger, with sizes ranging from 0.2 to 0.8 µm, whereas Ureaplasma tends to be smaller, measuring between 0.15 to 0.3 µm. A significant divergence emerges in their metabolic traits, with Ureaplasma’s ability to metabolize urea and produce ammonia setting it apart. Furthermore, Mycoplasma exhibits versatility in ecological niches, while Ureaplasma predominantly colonizes the urogenital tract. These distinctions are pivotal in understanding the unique roles these microorganisms play in the microbial world.
Introduction
Mycoplasma: The Tiny Titans
Mycoplasma, often referred to as “nature’s minimalists,” are remarkable bacteria known for their extraordinarily small size and unique features. They belong to the class Mollicutes and lack a rigid cell wall, making them distinct from most other bacteria. This absence of a cell wall gives them the flexibility to adopt various shapes, from spherical to filamentous, and enables them to squeeze through tight spaces, like the gaps between our body’s cells.
Characteristics of Mycoplasma
| Feature | Description |
|---|---|
| Cell Wall | Absent (lack a peptidoglycan cell wall) |
| Size | Among the smallest free-living bacteria (0.2 to 0.8 µm) |
| Motility | Exhibits gliding and twitching motility |
| Reproduction | Binary fission |
| Pathogenicity | Some species can cause human and animal diseases |
Ureaplasma: The Urea Utilizers
Ureaplasma, on the other hand, are unique in their ability to metabolize urea, a compound produced in the human body. These bacteria also belong to the class Mollicutes and share some similarities with Mycoplasma, such as lacking a cell wall. However, they have their own distinct characteristics that set them apart.
Characteristics of Ureaplasma
| Feature | Description |
|---|---|
| Cell Wall | Absent (lack a peptidoglycan cell wall) |
| Urea Metabolism | Can break down urea, producing ammonia |
| Size | Small, similar to Mycoplasma (0.15 to 0.3 µm) |
| Colonization | Commonly found in the human urogenital tract |
| Pathogenicity | Some strains associated with urinary and reproductive diseases |
Taxonomy and Classification
Mycoplasma Taxonomy
Mycoplasma is a diverse genus, with over 200 species identified to date. They are classified within the class Mollicutes, which encompasses bacteria that lack a cell wall. Mollicutes are further categorized into the order Mycoplasmatales, with Mycoplasma being one of the most well-known genera within this order.
Here is a simplified overview of Mycoplasma taxonomy:
- Domain: Bacteria
- Phylum: Tenericutes
- Class: Mollicutes
- Order: Mycoplasmatales
- Family: Mycoplasmataceae
- Genus: Mycoplasma
Ureaplasma Taxonomy
Ureaplasma is a genus with several species, some of which are capable of metabolizing urea. Taxonomically, Ureaplasma also falls within the class Mollicutes and the order Mycoplasmatales, similar to Mycoplasma.
Here’s an overview of Ureaplasma taxonomy:
- Domain: Bacteria
- Phylum: Tenericutes
- Class: Mollicutes
- Order: Mycoplasmatales
- Family: Mycoplasmataceae
- Genus: Ureaplasma
Morphology and Size
Mycoplasma Morphology
Mycoplasma bacteria are well-known for their distinct morphology. Their lack of a cell wall grants them an unusual, pleomorphic shape, allowing them to change from a spherical to filamentous structure based on environmental conditions. Despite their flexibility, they typically maintain a small size, with diameters ranging from 0.2 to 0.8 µm.
Ureaplasma Morphology
Ureaplasma shares a similar lack of a cell wall with Mycoplasma, resulting in a pleomorphic shape. These bacteria are also small, with a size range similar to Mycoplasma, typically between 0.15 to 0.3 µm.
In terms of morphology, the primary distinction between Mycoplasma and Ureaplasma lies in their ability to adapt to various shapes while remaining small and cell wall-free.
Metabolism and Urea Utilization
Mycoplasma Metabolism
Mycoplasma bacteria are chemoorganotrophs, which means they obtain energy from the metabolism of organic compounds. They lack the ability to metabolize urea, which is a key differentiating factor from Ureaplasma.
Ureaplasma Urea Utilization
Ureaplasma, as the name suggests, possesses a unique metabolic feature – the ability to metabolize urea. This distinctive trait sets Ureaplasma apart from Mycoplasma and many other bacteria. When Ureaplasma breaks down urea, it produces ammonia as a byproduct, which can affect the pH of its environment and potentially contribute to its pathogenicity in certain contexts.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Metabolism | Chemoorganotrophic | Urease-positive (urea metabolism) |
| Urea Utilization | Cannot metabolize urea | Metabolizes urea, produces ammonia |
Ecological Niches
Mycoplasma’s Ecological Niche
Mycoplasma species are incredibly versatile when it comes to ecological niches. They can be found in various habitats, including soil, plants, and animals. Some Mycoplasma species are pathogenic to humans and animals, causing diseases like pneumonia, urinary tract infections, and more. Others, however, are commensal, residing peacefully in their host’s body without causing harm.
Ureaplasma’s Ecological Niche
Ureaplasma primarily colonizes the urogenital tracts of humans. These bacteria are often present in the reproductive and urinary systems, and their colonization can be associated with certain health conditions. Ureaplasma’s affinity for the urogenital tract distinguishes it from Mycoplasma, which can have a broader ecological range.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Ecological Niche | Versatile, found in soil, plants, animals | Primarily colonizes the urogenital tract |
Pathogenicity and Human Health
Mycoplasma and Human Health
Mycoplasma species exhibit varied pathogenicity. Some Mycoplasma species are responsible for human diseases, including respiratory infections like Mycoplasma pneumoniae, which can lead to conditions such as atypical pneumonia. Other species can cause urogenital infections, arthritis, and more. Notably, Mycoplasma infections often present with symptoms that can be challenging to distinguish from those caused by other pathogens, making diagnosis and treatment more complex.
Ureaplasma and Human Health
Ureaplasma species, while less well-known than Mycoplasma, also have implications for human health. They are commonly associated with urinary and reproductive tract infections. Ureaplasma’s ability to metabolize urea and produce ammonia may contribute to its pathogenicity in these contexts. In some cases, Ureaplasma infections can lead to adverse pregnancy outcomes, making them of particular concern to pregnant individuals.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Pathogenicity | Causes respiratory, urogenital infections | Associated with urinary, reproductive infections |
| Pregnancy Risks | Generally not associated with adverse pregnancy outcomes | Associated with adverse pregnancy outcomes |
Diagnosis and Detection
Mycoplasma Diagnosis
Diagnosing Mycoplasma infections can be challenging due to the broad spectrum of symptoms they can cause and the need for specialized testing. Various methods are employed to detect Mycoplasma, including polymerase chain reaction (PCR), serological tests, and culture-based techniques. These diagnostic methods vary in sensitivity and specificity, and the choice often depends on the specific disease being investigated.
Ureaplasma Diagnosis
Diagnosing Ureaplasma infections follows a similar pattern to Mycoplasma. It can be difficult due to the non-specific symptoms they produce. Diagnosis typically involves molecular techniques like PCR, serological tests, and culture-based methods. However, it’s important to note that different Ureaplasma species can exist within the same host, making accurate diagnosis and treatment more complex.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Diagnosis | PCR, serological tests, culture-based techniques | PCR, serological tests, culture-based techniques |
Treatment and Antibiotic Susceptibility
Mycoplasma Treatment
The treatment of Mycoplasma infections typically involves antibiotics. However, Mycoplasma’s lack of a cell wall makes it inherently resistant to antibiotics that target cell wall synthesis, such as penicillins. Therefore, tetracyclines, macrolides, and fluoroquinolones are often the go-to choices for Mycoplasma infections. It’s crucial to choose the appropriate antibiotic based on the specific Mycoplasma species and the clinical context.
Ureaplasma Treatment
Ureaplasma infections are also treated with antibiotics, and they share the same challenge as Mycoplasma in terms of antibiotic susceptibility. The absence of a cell wall makes them less susceptible to cell wall-targeting antibiotics. Tetracyclines and macrolides are commonly used to treat Ureaplasma infections. However, it’s important to note that antibiotic resistance is a growing concern, and susceptibility patterns may vary among Ureaplasma strains.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Treatment | Antibiotics (tetracyclines, macrolides, fluoroquinolones) | Antibiotics (tetracyclines, macrolides) |
| Antibiotic Resistance | Growing concern | Variability in susceptibility patterns |
Genetic Diversity
Mycoplasma Genetic Diversity
Mycoplasma species exhibit a wide range of genetic diversity. Their genomes are relatively small compared to other bacteria, but they can still vary significantly in terms of gene content and organization. This genetic diversity is partly responsible for the different pathogenic potentials of Mycoplasma species. Some species, like Mycoplasma pneumoniae, have relatively larger genomes with numerous genes involved in host-pathogen interactions, while others, like Mycoplasma genitalium, have smaller genomes but still exhibit pathogenicity.
Ureaplasma Genetic Diversity
Ureaplasma species also display genetic diversity, which influences their pathogenicity and host specificity. The presence or absence of particular genes in Ureaplasma genomes can impact their ability to colonize and infect specific hosts, including humans. Understanding the genetic diversity of Ureaplasma is essential for deciphering its role in various diseases and the mechanisms underlying its urea metabolism.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Genetic Diversity | Varies in gene content and organization | Genetic diversity influences host specificity |
Evolutionary History
Mycoplasma’s Evolution
Mycoplasma’s evolutionary history is a subject of scientific intrigue. Their lack of a cell wall is thought to be an adaptation to parasitic lifestyles within host organisms. Mycoplasma species are believed to have evolved from Gram-positive bacteria, which still possess a cell wall. Over time, these bacteria underwent extensive reduction in genome size, losing many genes and metabolic pathways as they adapted to life within host environments.
Ureaplasma’s Evolution
Ureaplasma’s evolutionary history is closely tied to its ability to metabolize urea. This unique metabolic trait likely evolved as an adaptation to life within the urogenital tract of hosts. The exact origins of Ureaplasma and the timeline of its evolution are areas of ongoing research. Studying Ureaplasma’s evolutionary history can shed light on its role in host-microbe interactions.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Evolutionary History | Adaptation to parasitic lifestyles, loss of cell wall | Likely adaptation to urogenital tract, urea metabolism |
Environmental Resilience
Mycoplasma’s Environmental Resilience
Mycoplasma’s lack of a cell wall can be both an advantage and a challenge. Their flexibility in shape allows them to navigate tight spaces in host tissues, contributing to their ability to colonize various environments. However, their vulnerability to osmotic pressure and environmental changes can be a limiting factor. Mycoplasma species are often sensitive to desiccation and temperature fluctuations, making them more suited to parasitic lifestyles within host organisms.
Ureaplasma’s Environmental Resilience
Ureaplasma’s environmental resilience is also influenced by its lack of a cell wall. Its ability to colonize the urogenital tract and metabolize urea suggests a certain level of adaptability to specific host environments. However, like Mycoplasma, Ureaplasma can be sensitive to environmental changes, which may impact its survival outside the host.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Environmental Resilience | Flexibility in host colonization, sensitivity to environmental changes | Adaptability to host environments, sensitivity to environmental changes |
Research and Ongoing Studies
Mycoplasma Research
Mycoplasma research spans various fields, including microbiology, genomics, and medicine. Scientists continue to investigate the pathogenic mechanisms of different Mycoplasma species and are working on developing more effective diagnostic methods and treatments. Moreover, the study of Mycoplasma genomes provides insights into the genetic adaptations that have occurred during their evolution.
Ureaplasma Research
Ureaplasma research is also a dynamic area of study, with a focus on understanding the genetic diversity and pathogenicity of different Ureaplasma species. Scientists are actively researching the role of Ureaplasma in urogenital and reproductive tract infections, as well as its potential impact on pregnancy outcomes. Additionally, studies on Ureaplasma genomes are shedding light on the genetic factors contributing to its unique urea metabolism.
| Characteristic | Mycoplasma | Ureaplasma |
|---|---|---|
| Ongoing Research | Pathogenic mechanisms, diagnostics, treatments | Genetic diversity, host interactions, urea metabolism |
The Future of Mycoplasma and Ureaplasma Research
As we navigate through the intriguing world of microorganisms, it becomes clear that Mycoplasma and Ureaplasma are two genera of bacteria with unique characteristics and impacts on human and animal health. Research into these microorganisms continues to evolve, and our understanding of their biology, genetics, and pathogenicity deepens.
The future of Mycoplasma and Ureaplasma research holds exciting possibilities. Advances in genomics, microbiology, and biotechnology are likely to open new doors for studying these bacteria. Additionally, as antibiotic resistance becomes a growing concern, exploring alternative treatments and prevention strategies for Mycoplasma and Ureaplasma infections will be crucial.
In closing, we invite you to stay curious and engaged in the ever-evolving field of microbiology. Mycoplasma and Ureaplasma are just two examples of the countless microorganisms that shape our world. By delving into their unique characteristics, ecological niches, and impacts on human health, we continue to unravel the mysteries of the microbial realm, offering new insights and potential solutions to the challenges they present. Thank you for joining us on this journey through the world of Mycoplasma and Ureaplasma. We look forward to exploring more aspects of microbiology with you in the future.
FAQs
Mycoplasma and Ureaplasma are genera of bacteria belonging to the class Mollicutes. They are characterized by their lack of a peptidoglycan cell wall, making them unique among bacteria.
Mycoplasma is slightly larger, with sizes ranging from 0.2 to 0.8 µm, while Ureaplasma is smaller, typically measuring between 0.15 to 0.3 µm.
Mycoplasma exhibits gliding and twitching motility, whereas Ureaplasma does not display motility.
No, they differ significantly. Mycoplasma cannot metabolize urea, while Ureaplasma can break down urea, producing ammonia.
Mycoplasma is versatile and can be found in various habitats, including soil, plants, and animals. Ureaplasma primarily colonizes the urogenital tract in humans.
Some species of both Mycoplasma and Ureaplasma can be pathogenic. Mycoplasma species can cause various human and animal diseases, while certain Ureaplasma strains are associated with urinary and reproductive diseases.
Both Mycoplasma and Ureaplasma infections can be diagnosed using techniques such as PCR, serological tests, and culture-based methods.
Antibiotics are commonly used to treat both types of infections. Mycoplasma infections respond to tetracyclines, macrolides, and fluoroquinolones, while Ureaplasma infections are often treated with tetracyclines and macrolides.
Yes, antibiotic resistance is a growing concern for both Mycoplasma and Ureaplasma, with variations in susceptibility patterns.
Mycoplasma and Ureaplasma exhibit genetic diversity that influences their pathogenicity and host specificity. Their evolutionary history reflects adaptations to their respective ecological niches, such as parasitism and urogenital colonization.
Read More:
Contents
- Differences Between Mycoplasma and Ureaplasma
- Introduction
- Taxonomy and Classification
- Morphology and Size
- Metabolism and Urea Utilization
- Ecological Niches
- Pathogenicity and Human Health
- Diagnosis and Detection
- Treatment and Antibiotic Susceptibility
- Genetic Diversity
- Evolutionary History
- Environmental Resilience
- Research and Ongoing Studies
- The Future of Mycoplasma and Ureaplasma Research
- FAQs






